David Orchard-WebbJanuary 30, 2024
Tag: Hidradenitis Suppurativa treatment , Isotretinoin , Conventional therapies
Hidradenitis Suppurativa (HS) is a chronic inflammatory skin condition characterized by painful nodules, abscesses, and tunnels developing in areas where skin rubs together. A study found bacteria present in 49% of all Hidradenitis lesions, but they do not appear to be causative. [Jemec, 1996] [Ballard, 2024] Also known as acne inversa, this debilitating disease, thought to be present in 1-2% of people, often leads to severe scarring and has a significant impact on the quality of life for those affected. [Krueger, 2024] While conventional treatments such as anti-inflammatory medications including antibiotics with anti-inflammatory properties like topical clindamycin, and surgical interventions exist, there is growing interest in exploring the potential of vitamin treatments, including the use of Isotretinoin, except in pregnant women. [Nesbitt, 2020] Isoretinoin can potentially cause birth defects and its use is banned during pregnancy.
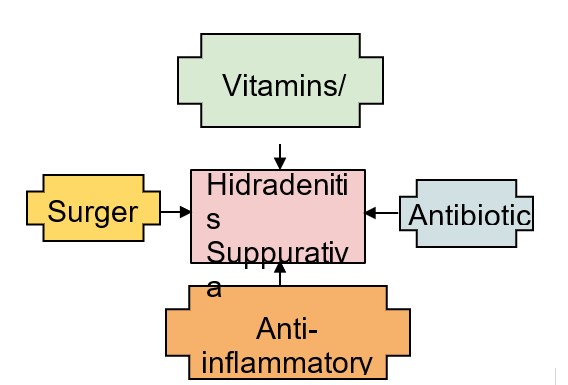
Figure: Treatment modalities for Hidradenitis Suppurativa
Notable conventional treatments and agents include:
1. Adalimumab: Two randomized phase III studies demonstrated the efficacy of adalimumab in the treatment of HS. Adalimumab targets tumor necrosis factor-alpha (TNF-α) and has been approved by both the FDA and EMA. [Kimball, 2016] [Krueger, 2024]
2. Secukinumab: In the largest phase III trials of HS to date, evaluating the IL-17A inhibitor secukinumab, the primary endpoint was met in the majority of settings, particularly moderate to severe HS. [Kimball, 2023] In October 2023, the FDA approved Cosentyx (secukinumab) to treat moderate to severe hidradenitis suppurativa (HS) in adults. [FDA, 2023]
3. Bermekimab: The LYRA study was underway to evaluate the failed cancer drug bermekimab, which targets interleukin-1 alpha (IL-1 alpha) and is an effective blocker of IL-1 alpha biological activity, for the treatment of moderate to severe HS. The interim analysis for efficacy, unfortunately, met the prespecified futility criteria and LYRA was terminated. [NCT04988308, 2021]
4. Spesolimab: A proof-of-concept safety study presented promising data for spesolimab an (IL-36R antagonist) in the treatment of HS. Spesolimab targets a specific mechanism related to HS pathophysiology, potentially normalizing cytokine signaling, immune cell activation, and neutrophil recruitment, and inhibiting hyperkeratosis to restore epithelial barrier function in the skin. [Joseph, 2022]
5. Lutikizumab: A phase II study is ongoing to assess the disease activity and safety of subcutaneous lutikizumab (an IL-1α/β inhibitor) in adult participants with moderate to severe HS who have failed anti-tumor necrosis factor therapy. [NCT05139602, 2021]
6. CSL324: Safety and pharmacokinetics of repeat doses of CSL324 recombinant anti-granulocyte colony-stimulating factor (G-CSF) receptor monoclonal antibody are being evaluated in subjects with HS and palmoplantar pustulosis, diseases that may be caused by increased numbers of neutrophils at sites of inflammation. [NCT03972280, 2019]
7. Bimekizumab: Bimekizumab, targeting IL-17A and IL-17F, showed clinically meaningful, deep and maintained response over 48 weeks in two Phase 3 studies (BE HEARD I and BE HEARD II). The EMA is reviewing a marketing application for bimekizumab in hidradenitis suppurativa. [UBC, 2023] [Healio, 2023]
8. Izokibep: A study is ongoing to evaluate Izokibep, a synthetic molecular trap targeting IL-17A/A, for the treatment of HS. [NCT05355805, 2022]
9. Spesolimab: The Phase IIa proof-of-clinical-concept study (NCT04762277) investigated the efficacy of spesolimab, an anti-IL-36 receptor monoclonal antibody, in patients with moderate-to-severe HS. The study showed that spesolimab was well-tolerated, resulting in a decrease in all HS lesions, supporting its development as a targeted therapy for HS. [Alavi, 2023]
These treatments and agents represent a diverse range of therapeutic targets, including cytokines and signal transduction pathways, and reflect the ongoing efforts to develop effective therapies for HS using advanced pharmaceuticals.
Vitamin A, a fat-soluble vitamin, plays a crucial role in maintaining healthy skin and mucous membranes. [ACS, 2024] It is involved in cell differentiation and helps regulate the immune system. Isotretinoin, a synthetic derivative of vitamin A, has been widely used in the treatment of severe acne due to its ability to reduce sebum production and prevent the formation of comedones. [AAD, 2023] Severe acne and HS differ mainly in the location of the lesions only, and so researchers have investigated whether Isotretinoin can be efficacious in managing HS symptoms as well.
Studies and Clinical Trials:
Several studies have explored the potential benefits of Isotretinoin in treating HS. One such study investigating the use of Isotretinoin in moderate to severe HS patients found that 36% (9/25 patients) demonstrated complete response to isotretinoin treatment.The study suggested that physicians should explore isotretinoin as a viable treatment for HS, as it may benefit individuals with mild to moderate condition, as well as patients who are female, younger, weigh less, and have a personal history of acne. [Huang, 2017]
Another retrospective review of HS patients at UCLA found a beneficial response to isotretinoin was reported by 14 (35.9%) patients. [Patel, 2021]
Vitamin D, known for its role in bone health, also plays a crucial role in immune modulation. Emerging evidence suggests that vitamin D deficiency may contribute to the pathogenesis of inflammatory skin conditions, including HS. Researchers are investigating whether vitamin D supplementation could be a viable option for managing HS symptoms by modulating the immune response. [Shen, 2023]
V. Omega-3 Fatty Acids and Anti-Inflammatory Effects:
Omega-3 fatty acids, commonly found in fish oil, have well-established anti-inflammatory properties. [Yates, 2014] Given the inflammatory nature of HS, researchers are aware of the potential of omega-3 supplementation in managing HS symptoms, however no studies have directly assessed omega supplementation in the context of HS. These fatty acids may help regulate the immune response and reduce inflammation, offering a complementary approach to traditional treatments.
The complex nature of HS suggests that a multifaceted treatment approach may be most effective. Combining vitamin treatments, such as Isotretinoin, with other interventions like antibiotics, anti-inflammatory medications, and lifestyle modifications could provide a synergistic effect. For example, isotretinoin/ spironolactone has shown promise in mild HS as has isotretinoin or doxycycline with adalimumab in moderate disease. [McPhie, 2019]
While the preliminary results are promising, it is essential to acknowledge the challenges and considerations associated with vitamin treatments for HS.
Sporadic Efficacy: Isotretinoin has shown effectiveness in only 36% of HS patients. Developing biomarkers for these 36% of responders is therefore desirable.
Side Effects: Isotretinoin is associated with several side effects, including rheumatic effects and rarely sacroiliitis. [Coskun, 2019]
Worsening Symptoms: paradoxically isotretinoin can make HS symptoms worse and therefore treatment needs to be monitored closely by a healthcare professional. [Coskun, 2019]
Risk of Birth Defects: Isotretinoin is notorious for its potential to cause birth defects. [Nesbitt, 2020]
Patient variability, potential side effects, and the need for personalized approaches underscore the importance of ongoing research and close medical supervision.
In conclusion, Hidradenitis Suppurativa (HS) poses a significant challenge for patients due to its chronic and debilitating nature. Current conventional anti-inflammatory treatments, such as Adalimumab, Secukinumab, Bermekimab, Spesolimab, Lutikizumab, CSL324, Bimekizumab, Izokibep, and ongoing research with other agents, reflect the diverse therapeutic approaches targeting cytokines and signal transduction pathways. Vitamin treatments, particularly Isotretinoin, have shown promise in managing HS, but challenges such as sporadic efficacy, side effects, and the risk of birth defects highlight the need for careful consideration and personalized approaches. Ongoing research into vitamin D, omega-3 fatty acids, and combination therapies adds to the evolving landscape of potential treatments for HS. Despite the complexities and challenges, the pursuit of effective therapies for Hidradenitis Suppurativa remains a crucial area of focus to improve the lives of those affected by this condition.
AAD, "Isotretinoin: Overview" American Academy of Dermatology Association. , 12 Sep. 2023, online, Internet, 29 Jan. 2024. , Available: https://www.aad.org/public/diseases/acne/derm-treat/isotretinoin.
ACS, "Vitamin A and Retinoic acid" American Chemical Society. , n.d., online, Internet, 29 Jan. 2024. , Available: https://www.acs.org/molecule-of-the-week/archive/v/vitamin-a.html.
Alavi, Afsaneh et al., "Spesolimab for Hidradenitis Suppurativa: A Proof-of-Concept Study" SKIN The Journal of Cutaneous Medicine. 7.6 (2023): s286, online, Internet, 28 Jan. 2024. , Available: https://jofskin.org/index.php/skin/article/view/2427.
Ballard, Kimberly, and Victoria L. Shuman, "Hidradenitis Suppurativa" in StatPearls. , vols. (Treasure Island (FL): StatPearls Publishing, 2024), online, Internet, 26 Jan. 2024. , Available: http://www.ncbi.nlm.nih.gov/books/NBK534867/.
Coskun, Belk?s Nihan et al., "Isotretinoin-induced sacroiliitis in patients with hidradenitis suppurativa: a case-based review" Rheumatology International. 39.12 (2019): 2159-2165, online, Internet, 29 Jan. 2024. , Available: http://link.springer.com/10.1007/s00296-019-04434-1.
"FDA approves Novartis Cosentyx? as the first new biologic treatment option for hidradenitis suppurativa patients in nearly a decade" Novartis United States of America. , 31 Oct. 2023, online, Internet, 26 Jan. 2024. , Available: https://www.novartis.com/us-en/news/media-releases/fda-approves-novartis-cosentyx-first-new-biologic-treatment-option-hidradenitis-suppurativa-patients-nearly-decade.
Healio, "EMA accepts marketing authorization for bimekizumab for hidradenitis suppurativa," 18 Jul. 2023, online, Internet, 27 Jan. 2024. , Available: https://www.healio.com/news/dermatology/20230718/ema-accepts-marketing-authorization-for-bimekizumab-for-hidradenitis-suppurativa.
Huang, Christina M. and Mark G. Kirchhof, "A New Perspective on Isotretinoin Treatment of Hidradenitis Suppurativa: A Retrospective Chart Review of Patient Outcomes" Dermatology. 233.2-3 (2017): 120-125, online, Internet, 29 Jan. 2024. , Available: https://www.karger.com/Article/FullText/477207.
Jemec, G.B.E. et al., "The Bacteriology of Hidradenitis suppurativa" Dermatology. 193.3 (1996): 203-206, online, Internet, 28 Jan. 2024. , Available: https://www.karger.com/Article/FullText/246246.
Joseph, David et al., "Assessment of the Pharmacokinetics and Safety of Spesolimab, a Humanised Anti-interleukin-36 Receptor Monoclonal Antibody, in Healthy Non-Japanese and Japanese Subjects: Results from Phase I Clinical Studies" Clinical Pharmacokinetics. 61.12 (2022): 1771-1787, online, Internet, 26 Jan. 2024. , Available: https://link.springer.com/10.1007/s40262-022-01176-5.
Kimball, Alexa B., et al., "Secukinumab in moderate-to-severe hidradenitis suppurativa (SUNSHINE and SUNRISE): week 16 and week 52 results of two identical, multicentre, randomised, placebo-controlled, double-blind phase 3 trials" The Lancet. 401.10378 (2023): 747-761, online, Internet, 26 Jan. 2024. , Available: https://linkinghub.elsevier.com/retrieve/pii/S0140673623000223.
Kimball, Alexa B., et al., "Two Phase 3 Trials of Adalimumab for Hidradenitis Suppurativa" New England Journal of Medicine. 375.5 (2016): 422-434, online, Internet, 26 Jan. 2024. , Available: http://www.nejm.org/doi/10.1056/NEJMoa1504370.
Krueger, James G., et al., "Hidradenitis suppurativa: new insights into disease mechanisms and an evolving treatment landscape" British Journal of Dermatology. 190.2 (2024): 149-162, online, Internet, 26 Jan. 2024. , Available: https://academic.oup.com/bjd/article/190/2/149/7275339.
McPhie, Meghan L, Alanna C. Bridgman, and Mark G. Kirchhof, "Combination Therapies for Hidradenitis Suppurativa: A Retrospective Chart Review of 31 Patients" Journal of Cutaneous Medicine and Surgery. 23.3 (2019): 270-276, online, Internet, 29 Jan. 2024. , Available: http://journals.sagepub.com/doi/10.1177/1203475418823529.
NCT03972280, Safety and Pharmacokinetics of Repeat Doses of CSL324 in Subjects With Hidradenitis Suppurativa and Palmoplantar Pustulosis, Clinical Trial, vols., July 4, 2019, online, Internet, 26 Jan. 2024. , Available: https://clinicaltrials.gov/study/NCT03972280.
NCT04988308, A Study of Bermekimab for the Treatment of Participants With Moderate to Severe Hidradenitis Suppurativa (LYRA), Clinical Trial, vols., October 12, 2021, online, Internet, 26 Jan. 2024. , Available: https://clinicaltrials.gov/study/NCT04988308.
NCT05139602, A Study to Assess Disease Activity and Safety of Subcutaneous Lutikizumab (ABT-981) in Adult Participants With Moderate to Severe Hidradenitis Suppurativa Who Have Failed Anti-Tumor Necrosis Factor (TNF) Therapy and Who Are Na?ve to Biologic Therapy, Clinical Trial, vols., December 28, 2021, online, Internet, 26 Jan. 2024. , Available: https://clinicaltrials.gov/study/NCT05139602.
NCT05355805, Hidradenitis Suppurativa Phase 2b Pivotal Study of Izokibep, Clinical Trial, vols., May 5, 2022, online, Internet, 27 Jan. 2024. , Available: https://clinicaltrials.gov/study/NCT05355805.
Nesbitt, Emily, Stephanie Clements, and Marcia Driscoll, "A concise clinician's guide to therapy for hidradenitis suppurativa" International Journal of Women's Dermatology. 6.2 (2020): 80-84, online, Internet, 29 Jan. 2024. , Available: https://linkinghub.elsevier.com/retrieve/pii/S2352647519301224.
Patel, Nirali, et al., "Isotretinoin in the treatment of hidradenitis suppurativa: a retrospective study" Journal of Dermatological Treatment. 32.4 (2021): 473-475, online, Internet, 29 Jan. 2024. , Available: https://www.tandfonline.com/doi/full/10.1080/09546634.2019.1670779.
Shen, Alan S. Jessica S. Johnson, and Michelle Lynn Kerns, "Dietary Factors and Hidradenitis Suppurativa" Dermatology and Therapy. 13.12 (2023): 3007-3017, online, Internet, 29 Jan. 2024. , Available: https://link.springer.com/10.1007/s13555-023-01056-1.
UCB, "Bimekizumab Phase 3 Data in Hidradenitis Suppurativa Show Clinically Meaningful, Deep and Maintained Response over 48 Weeks," 18 Mar. 2023, online, Internet, 26 Jan. 2024. , Available: https://www.ucb.com/stories-media/Press-Releases/article/Bimekizumab-Phase-3-Data-in-Hidradenitis-Suppurativa-Show-Clinically-Meaningful-Deep-and-Maintained-Response-over-48-Weeks.
Yates, Clara M, Philip C. Calder, and G. Ed Rainger, "Pharmacology and therapeutics of omega-3 polyunsaturated fatty acids in chronic inflammatory disease" Pharmacology & Therapeutics. 141.3 (2014): 272-282, online, Internet, 29 Jan. 2024. , Available: https://linkinghub.elsevier.com/retrieve/pii/S0163725813002155.
David Orchard-Webb, Ph.D., is a technical writer with broad interests including health & technology writing, plus extensive training and knowledge of biomedicine and microbiology. My Ph.D. and postdoc were in oncology and developing cancer medicines. I provide technical medical and other writing services for projects ranging from “knowledge automation” to pure pharma, to food safety, to the history of science, and everything in between. I also provide white papers, ebooks, meta-analysis reviews, editing, consulting, business, and market research-related activities in biomedicine, technology, and health. In addition to its well-known role in the development of medicines, I am a big believer in biotechnology’s ability to revolutionize industries such as food-tech, agtech, textiles & fashion.


Contact Us
Tel: (+86) 400 610 1188
WhatsApp/Telegram/Wechat: +86 13621645194
Follow Us:




 Pharma Sources Insight January 2025
Pharma Sources Insight January 2025


